Remote patient monitoring (RPM/RTM) represents an exciting opportunity for providers and practices to improve patient outcomes, lower costs, improve patient satisfaction & engagement, and increase provider revenue. Everyone benefits.
Topics: transforming healthcare, value-based care, remote patient monitoring
Remote Physiologic Monitoring devices provide care teams with both longitudinal and acute data to facilitate intervention at critical points, which leads to the RPM industry’s core metrics of avoidance of hospitalizations or readmissions after an acute episode. These are huge cost drivers, but are those really the targets we should be shooting for? I don’t think so, but existing RPM solutions are not built to deliver more. Ultimately, remote care solutions, including RPM, should first seek to change behavior and lower risk, then seek to intervene in acute episodes as needed. We need to rethink RPM.
RPM should be a component of a larger Remote Care Platform, RCP. Here are our core truths related to this topic.
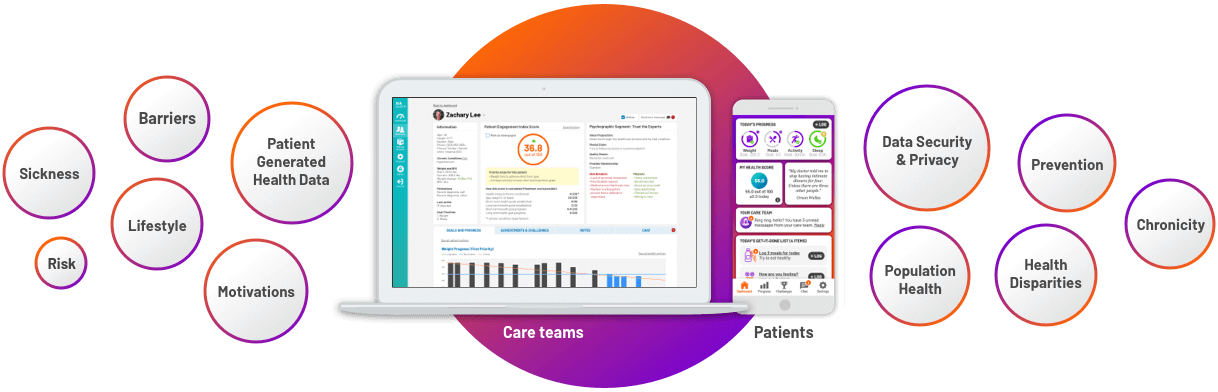
- Remote monitoring should primarily be embedded in a larger remote care technology platform and strategy. Remote care focuses on patient generated data beyond just device data including diet, exercise/activity, mood, sleep, medication and care plan adherence, etc. The individual’s weight, blood pressure, blood glucose, oxygen saturation, and/or lung function data from the RPM device is then contextualized to the modifiable risk factor data supporting patient behavior change and opening the door for clinicians to get at root cause behaviors. With remote care, behavior change is a critical factor.
- Remote care platforms should drive/facilitate efficient and effective interaction between the care team and the patient. RPM solutions today are almost exclusively unidirectional. Data flows from the device to the care team and to coding for billing purposes. Interaction happens through other disconnected channels and is based solely on the existence of device readings. An out-of-range reading will trigger an alert-based interaction, but there is no context to the reading and the interaction is by its nature reactive. Remote care includes integrated communication channels. Platforms should facilitate proactive interaction efficiently and effectively, not just for the purpose of time tracking and CPT code submission.
- Remote care platforms should incorporate health disparity information, personal barriers, and individual motivations in a goal-based structure. Just knowing and establishing device reading parameters is insufficient. Remote care and monitoring platforms should capture personal patient environmental and motivational variables and facilitate goal setting between the two parties. Then they should bring this critical data (outside of just device readings) directly into the care team workflow.
- Finally, based on these, we should be measuring patient health outcomes tied to healthy behaviors, the reduction of risk and chronicity, health goal attainment, as well as device reading parameters. Yes, today we can avoid hospitalizations and readmissions by over 60%, which is a great start, but also not enough. We need to focus on how we are changing the health trajectory of patients.
Andrew Richburg-CEO
As a global digital health company, we are excited to join StartUp Health on their mission to improve the health and wellbeing of everyone in the world. They open doors and increase our voice to health systems, partners, and investors. It is a critical time for us, and with StartUp, we could not be more thrilled about our future. StartUp Health recently introduced us to their community, by featuring C3LX in their newsletter explaining why they chose to invest in our mission.
Topics: healthcare technology, transforming healthcare, value-based care
C3LX Inc partners with athenahealth’s Marketplace Program to help value-based and Direct Primary Care practices remotely monitor patients, increase patient engagement, and achieve superior outcomes.
Topics: healthcare technology, transforming healthcare, value-based care
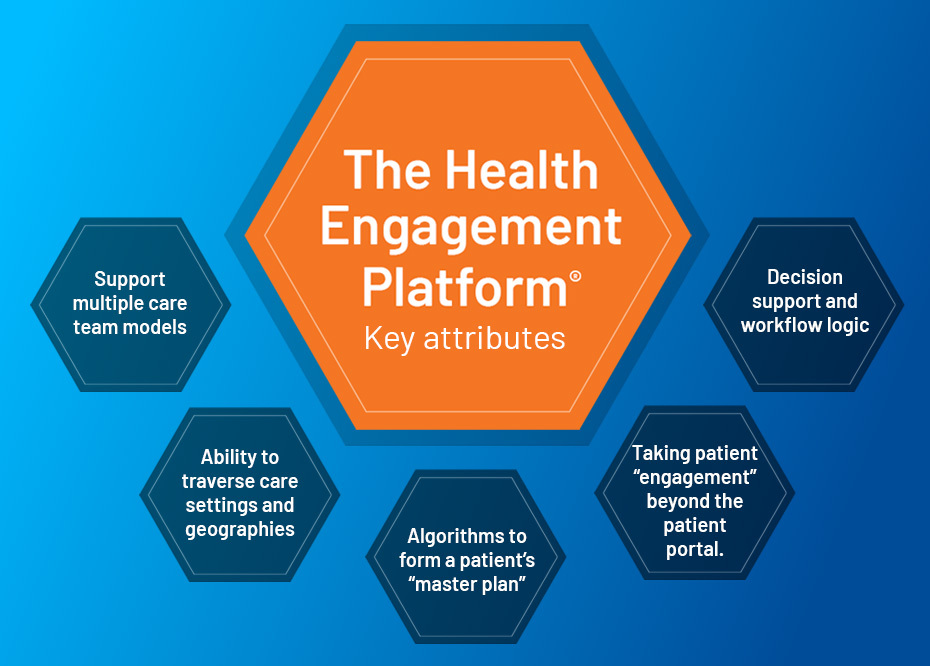
Recently, we’ve been sharing our vision for a technology platform that transforms the EHR beyond merely a digital documentation tool into a platform that empowers patients and clinicians towards improving health; both at an individual level and across a population. In order to achieve this vision, what are the key attributes and elements of this new comprehensive platform? Below is a summary of how we, at C3LX, are reimagining healthcare technology:
Topics: healthcare technology, transforming healthcare, value-based care
Patients rarely have just one clear, manageable issue. Even more importantly, people are multi-faceted, complex, and cannot be broken down to the presence or absence of a chronic condition or comorbidity. C3LX is building towards a comprehensive solution that allows care teams to work with individual patients to create a master plan that addresses all facets of their health journey; from treating a patient’s asthma, arthritis, depression and weight loss, while simultaneously understanding the intrinsic motivations and potential barriers affecting the necessary underlying behavioral changes.
Topics: healthcare technology, transforming healthcare, value-based care
It’s time for your EHR to be more than a documentation and decision support tool, and finally become the essential platform in driving effective and efficient care and interaction with your patients, regardless of the setting.
Topics: healthcare technology, transforming healthcare, value-based care
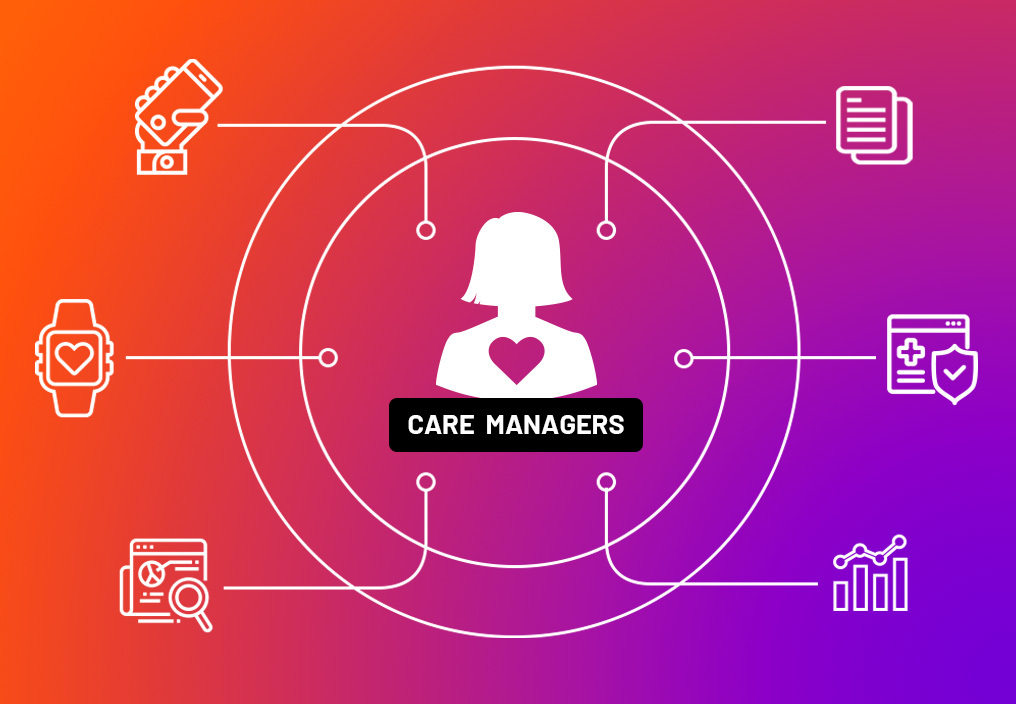
Digital Health Capabilities to Effectively Support Value-Based Care: Tools for Care Managers
Care managers who support patient populations and other providers are critical for successful value-based models. Typically care managers are either a part of a diverse care team within an individual practice or they function as a centralized unit providing wrap-around support for patient populations spanning multiple practices. Unlike the workflow of the physicians within a practice that tend to focus on the patient in front of them or the schedule for the day, care managers can take a more proactive view looking ahead at patients that require more active attention and dynamic engagement.
Topics: healthcare technology, transforming healthcare, value-based care
Digital Engagement is Here to Stay - Embracing Patient-Centric Technology
The use of telehealth rapidly increased during the spring as it gave patients a needed way to connect with their physician and reimbursement restrictions were lifted. During this time of a rapid increase in adoption, patients as consumers expect more from their digital tools and compare their experiences to offerings from other industries. Notably, as we head into fall, already the usage of telehealth offerings is declining as physician practices open back up and patients feel safer to return to in-person visits.
Topics: healthcare technology, transforming healthcare, patient engagement, telehealth
- Scheduling appointments, refilling prescriptions and looking up lab results are important, but true engagement comes first in understanding unique patient needs, wants, motivations and barriers to achieving care goals and the lifestyle changes needed to be successful; and then in supporting patients along the journey to achieving those goals.
- Patients rarely have just one, clear, manageable issue. A smart platform would take in a variety of inputs and combine appropriate algorithms for treating a patient’s asthma, arthritis, depression, and weight reduction without the clinician having to synthesize these disparate data points on their own.
- Each care team member is able to see both the patient’s master plan and the relevant data and prioritization that is specific to their role and scope of practice. With the growing dynamic of team-based care, each member has a personalized dynamic dashboard to work in.
- The master plan and supportive tools need to travel seamlessly with the patient, whether they are at home with devices tracking their activity, sleep, and blood pressure; or on the road for work or play, even when seeing a specialist. The primary care team then needs the relevant data and information to come back to them through the platform in meaningful and actionable ways.
- The platform must remind care team members and patients of upcoming and overdue activities, suggest changes in the master plan when patient conditions and care needs change, and route messages to the appropriate care team member regarding new test results, data trends negatively, or when patient health goals aren’t on track or being met. All of these long before an adverse event occurs.
At scale, the Health Engagement Platform facilitates the thousands of master plans seamlessly, undergirds a myriad of patient/provider workflows, simultaneously traverses multiple care settings, and supports hundreds of thousands of highly personalized provider decisions; so that a population can be proactively managed as never before. This is the future of healthcare technology!
Topics: healthcare technology, transforming healthcare, patient engagement